A System To Help More Patients Receive Care for Active Periodontal Disease in the Era of Saliva Testing
(This post is lengthy, click on link for printable copy) Whitepaper-Active Periodontal Disease in the Era of Saliva Testing
Dentists across the country are failing their patients daily. This failure is not one of neglect, or for lack of trying. This failure is one helping our patients travel the path from UNAWARE to ACTION. Altering the perceived importance of treating a disease that not only destroys the bone support of teeth but also contributes to a weakening of the luminal wall of their arteries that could lead to heart attack or stroke is not only a strategic imperative for your business but a moral imperative as well. Every day, most dentists diagnose periodontitis, and every day one out of two people who hear about their periodontal disease decide not to pursue a treatment that can save their teeth and potentially their life.
The purpose of this white paper is to discuss a system designed to help patients move from a lack of awareness to awareness and then to belief. Once a belief is changed in the presence of an acknowledged self-interest the patient can establish a commitment to health and ultimately to an action. New technologies combined with old techniques can save teeth and lives. New technologies such as the MyPerioPath test from Oral DNA Labs and time-tested behavioral understanding such as the “learning ladder” combined with proven diagnosis techniques such as co-discovery can transform the acceptance of care and significantly impact the health of your patient base. The system is not difficult, but it is hard. The system is hard because it takes an investment of time and a variable investment in patience to help patients move from unaware to action and skipping steps is folly that will result in fewer people accepting your finest and best care. With a dedication to helping patients travel the journey with compassion and empathy, we can improve the lives of more of our patients than our current systems allow.
The Problem:
Most of the time dental disease does not hurt at the early stages of the disease. Most people don’t spend a lot of time inspecting their mouth or doing much more than brushing their teeth. The lack of visible and noticeable signs of a disease means that most patients are unaware of their oral condition. Lack of awareness of the public coupled with an inconsistent emphasis on periodontal health among dental professionals has led to a preponderance of disease left untreated in the general population. The CDC has reported that 48% of adults over 30 have at least some evidence of active or previously active periodontal disease. Trust is lost among patients as more dentists begin to attempt to treat periodontal disease through the use of “The Expert Model.” The expert model is where awareness is made simply through telling the patient they have the disease. Combine a truncated patient process, to a relatively high fee compared to what the patient perceives to be the appropriate treatment (prophy,) the dental office is lucky to experience a 50% case acceptance. The shortened patient process is moving from unawareness to awareness to action without first attempting to obtain an acknowledged self-interest, an attitude and or belief change and a commitment to improving their oral health.
The Solution (Behavioral Science Combined with Laboratory Testing)
The days of being able to say, “you have it, I can fix it” are gone in dentistry. Today, we must demonstrate patience and empathy with our patients as they move through the process. The behavioral component of the solution is not new, just not widely implemented by dental professionals.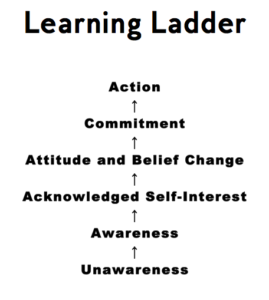 The lack of adoption of the behavioral process is due to a combination of lack of knowledge and the amount of time and skill development for the provider needed to implement the system. Co-discovery and motivational interviewing have been around for decades and championed primarily by the highest end fee-for-service segment of our profession. The fact that this niche of the industry has embraced these skill sets is no wonder because these providers have a more limited patient base and it is much more critical for their practice survival that they master the skill set of getting people to say yes. It is unfortunate that many in-network providers have not embraced the necessary skill set because it can help move all patients regardless of payer mix toward action. What is “Co-discovery” and “Motivational Interviewing” and how precisely can they be used in periodontal disease?
The lack of adoption of the behavioral process is due to a combination of lack of knowledge and the amount of time and skill development for the provider needed to implement the system. Co-discovery and motivational interviewing have been around for decades and championed primarily by the highest end fee-for-service segment of our profession. The fact that this niche of the industry has embraced these skill sets is no wonder because these providers have a more limited patient base and it is much more critical for their practice survival that they master the skill set of getting people to say yes. It is unfortunate that many in-network providers have not embraced the necessary skill set because it can help move all patients regardless of payer mix toward action. What is “Co-discovery” and “Motivational Interviewing” and how precisely can they be used in periodontal disease?
Co-discovery
Bob Barkley is the founder of the movement to allow people to participate in the process of learning about their condition. Dr. Barkley did this primarily with a hand mirror and patience. The system of co-discovery as it relates to periodontal health is simple enough. First, teach your patient what healthy looks like by showing them. I still like a hand mirror. I place the hand mirror in their hand and invite them to look at their anterior teeth with me. The maxillary anterior are easy to see and in most patients are relatively healthy. Patients cannot appreciate disease until they know what healthy looks like. I like to use a simple probe that is yellow and black and segmented 3-6-9-12 because it is easy for the patient to see and follow. My language: “Now I’m going to see how healthy your gums are. Let me show you how I check your gums. This instrument next to your tooth is like a ruler. Can you see how it changes from yellow to black? Now look at this tooth. Can you see how pink the gum tissue is here? Can you see how when I place the instrument next to the gum the tip goes in between the gum and the tooth? Can you feel how at this point it meets resistance? I couldn’t make this go any deeper without it hurting. Where you feel the resistance is the point where you gum connects to your tooth. In this spot it is 2mm. 1, 2, and 3 mm are considered healthy. Can you see when I take the instrument away from the gum that it does not bleed? That is also a sign of health. The gums around this tooth are healthy. If I see anywhere that is not healthy I would like to show you what that looks like in your mouth. Is that ok?” Next, I move to the most distal site in the upper right quadrant and proceed like normal. The moment I encounter any deviation from health I re-engage the patient and invite them to discover what I am discovering. When a patient knows what health is, they can appreciate disease. Patients achieve awareness when they see disease in their mouth.
My language: “Now I’m going to see how healthy your gums are. Let me show you how I check your gums. This instrument next to your tooth is like a ruler. Can you see how it changes from yellow to black? Now look at this tooth. Can you see how pink the gum tissue is here? Can you see how when I place the instrument next to the gum the tip goes in between the gum and the tooth? Can you feel how at this point it meets resistance? I couldn’t make this go any deeper without it hurting. Where you feel the resistance is the point where you gum connects to your tooth. In this spot it is 2mm. 1, 2, and 3 mm are considered healthy. Can you see when I take the instrument away from the gum that it does not bleed? That is also a sign of health. The gums around this tooth are healthy. If I see anywhere that is not healthy I would like to show you what that looks like in your mouth. Is that ok?” Next, I move to the most distal site in the upper right quadrant and proceed like normal. The moment I encounter any deviation from health I re-engage the patient and invite them to discover what I am discovering. When a patient knows what health is, they can appreciate disease. Patients achieve awareness when they see disease in their mouth.
“When a patient knows what health is, they can appreciate disease. Patients achieve awareness when they see disease in their mouth.”
Motivational Interviewing
If patients all shared our knowledge and were self-motivated to get better, our job would be easier. Unfortunately, most patients neither know what we know nor care as much as we do. Interviewing patients in a way that allows the provider to connect with a patient on a level deeper than rapport is a fundamental advantage of motivational interviewing. One of the goals of motivational interviewing is to establish a mutually trusting and respectful helping relationship. In his book “Motivational Interviewing in Dentistry” Dr. Lynn Carlisle thoroughly outlines the processes of engaging, focusing, evoking and planning and provides conversation tools such as open questions, affirmations, reflections, and summarizations. Dr. Carlisle also provides insight on how to avoid the common traps such as the assessment trap, the expert trap, premature focus, labeling trap, blaming trap and the chat trap. Mastering motivational interviewing is a process that takes time and practice. I recommend reading Dr. Carlisle’s book for greater insight.
In his book “Motivational Interviewing in Dentistry” Dr. Lynn Carlisle thoroughly outlines the processes of engaging, focusing, evoking and planning and provides conversation tools such as open questions, affirmations, reflections, and summarizations. Dr. Carlisle also provides insight on how to avoid the common traps such as the assessment trap, the expert trap, premature focus, labeling trap, blaming trap and the chat trap. Mastering motivational interviewing is a process that takes time and practice. I recommend reading Dr. Carlisle’s book for greater insight.
Laboratory Testing:
The behavioral piece is important but how do you create awareness when the patient has a glimmer of distrust? Obviously, the co-discovery of a periodontal probe slipping past the point they now understand as healthy to something worse is important, but there is nothing like third party validation to help patients gain trust in the diagnosis. Advances in saliva diagnostics have allowed Oral DNA Labs to create a test that takes a sample of a patient’s saliva and identifies the specific pathogens that exist in their mouth. Oral DNA Labs provides a patient-friendly report that can be used to educate the patients about the bacteria that is present in their mouth and the risks associated with those bacteria. Combining the awareness of the bacteria with the knowledge of how different bacteria can contribute to systemic health dangers and aggressive bone loss helps patients acknowledge their self-interest in removing these bacteria from their mouth. Informing the patient that it is possible to eliminate the cause of their disease and that we can verify with testing that our efforts have been successful is helpful. This understanding provides the dentist or hygienist a better chance of creating an attitude and belief change about the condition of their mouth and what role the provider can have in their movement from disease to health. The MyPerioPath test is a powerful way to show patients that their future is not one of fate but one of choice. When patients move from helpless to hopeful commitment becomes possible. Commitment is not a given, remember, bacterial changes are not an event, but rather bacterial changes result from a process of daily behavior changes in conjunction with a variety of professional services, and support.
“The MyPerioPath test is a powerful way to show patients that their future is not one of fate but one of choice. When patients move from helpless to hopeful commitment becomes possible.”
Caveat: Some people don’t want to get better or are not in a position emotionally or financially to become aware. These patients frustrate dentists because the dentist assumes if they show up for an appointment they want to learn about their condition and if possible treat it. This assumption is not always correct. Some patients are comfortable with ambivalence and don’t want to exert the energy to leave the comfortable chair of ambivalence. Every provider must decide how to handle these patients. Certainly, it is within the rights of the dentist or hygienist to choose not to accept these patients where they are and drive them away overtly or covertly. I would encourage you to take the patients however they present. Continue to provide them opportunities to engage in the process and humbly inquire to gain understanding. Remember Stephan Covey’s fifth habit: seek first to understand and that with people slow is fast and fast is slow. If a patient is unwilling to purchase the test, chances are they will not want to buy much else. It is my recommendation that we attempt to offer them still the basic service of scaling and root planning in those sites with active disease and clinical attachment loss. Here we are doing the bare minimum and providing them a moment of health. The chances are high that you will still fail in your effort. Do not dress up you care with additional value added services, just offer the basic level of care and do it in a way that demonstrates your understanding of their unique situation and embraces them and their desires.
The System:
Pre-clinical Conversation/History
Before beginning any examination, it is important to engage the patient and learn what brought them in as well as determine what significant history they have that might be related to their oral condition. One provoking question is first to ask the patient to score themselves from 1-10, 10 being in perfect oral health and 1 being an abysmal oral condition. After they have scored themselves, follow up quickly by asking what level they would hope to achieve. If they answer “the same,” it is unlikely that you will convince the patient of the need for much of anything, especially at your first encounter.
Co-discovery examination
Co-discovery is easy to learn and implement. You can start today. (See above for a detailed example)
Preliminary diagnosis
After you have cataloged the patient’s oral condition, you can make a diagnosis of the condition based on physical and radiographic evidence. You will not be able to determine the particular causative factor at your examination appointment. A saliva sample test is the only way to identify the causative bacteria.
Testing
Each provider needs to decide for himself or herself how they want to engage patients around saliva testing. My language: “Based on what we just observed together I know you have periodontal disease, an infection in your gums. Bacteria living in your mouth cause this disease. Hundreds of different types of bacteria live in our mouths, what I don’t know is the specific bacteria that is causing your infection. If we can determine the type of bacteria causing your infection, I can better customize my care to your unique situation. The goal of treatment is to reduce the levels of the harmful bacteria to a level that they will not cause further harm. Dentistry has now advanced to the point where we can take a sample of your saliva and send it to a medical laboratory, and they will send us a report cataloging the bacteria that are causing your infection. This report will help us do two things; first, determine if you have any of the dangerous bacteria and secondly provide us a way to ensure successful outcomes. Additionally, Some of the bacteria that cause gum disease also travel into your blood stream and can weaken the walls of your arteries. A weakened arterial wall can cause a rupture and blood clot to form. If a blood clot forms in an artery and dislodges and goes to the heart, it can cause a heart attack, if it goes to the brain it can cause a stroke. Many other systemic issues can result from specific bacteria; this test will help us know where the risks are for you. The second thing the test will do is to allow us to determine how effective our treatment has been in the future. Unfortunately, dental insurance does not currently cover this test. The cost is $##. We have made the decision just to charge you the amount the laboratory charges us. Is this something you would like us to do today?” If yes: “fantastic, it usually takes about a week to get the results back. Today, we are going to do a general cleaning of your teeth, after we get the results back I will look at them and come up with a couple of options to treat this infection. Let’s set you up with an appointment next week to review the results.
Consultation/Commitment
The consultation appointment is designed to reinforce awareness, acknowledged self-interest, foster an attitude and belief change so that we can earn a commitment to action. If the co-discovery examination and motivational interviewing have been done well ahead of the consultation, this appointment will not take much time – ten minutes on average.  Oral DNA Labs has created a visually enticing report that explains things well. The OARS skills of motivational interviewing come in handy here. It is best to start with Open Questions such as “What questions have entered your mind about your periodontal disease since our last conversation” Summarizations are perhaps the most powerful. “I know you are concerned that you might have the bacteria that are associated with heart attacks because your father had a heart attack when he was your age and you are taking cholesterol medication.” Before asking for the commitment, you want to demonstrate the problem and explain the proposed solutions. Here you get to talk about SRP, systemic or localized antibiotic therapy, laser therapy, and the importance of quality oral hygiene. Based on what you have learned from your patient and the saliva test the doctor should create a package of services that he or she recommends. It is advised to include how you will ensure that you are getting results and how you and the patient agree to encourage and support continued home care. I want patients to have the perception that they are paying for a result, not a service. After all, no one wants to purchase scaling and root planning. People want to buy a better oral health future. For this reason, I make my treatment options time bound and make a commitment to them that if they are doing their part that we will add treatment at no additional cost over a predetermined amount of time until we deliver the results they are seeking. I think it is easier for them to commit to treatment when they know we are committed to them.
Oral DNA Labs has created a visually enticing report that explains things well. The OARS skills of motivational interviewing come in handy here. It is best to start with Open Questions such as “What questions have entered your mind about your periodontal disease since our last conversation” Summarizations are perhaps the most powerful. “I know you are concerned that you might have the bacteria that are associated with heart attacks because your father had a heart attack when he was your age and you are taking cholesterol medication.” Before asking for the commitment, you want to demonstrate the problem and explain the proposed solutions. Here you get to talk about SRP, systemic or localized antibiotic therapy, laser therapy, and the importance of quality oral hygiene. Based on what you have learned from your patient and the saliva test the doctor should create a package of services that he or she recommends. It is advised to include how you will ensure that you are getting results and how you and the patient agree to encourage and support continued home care. I want patients to have the perception that they are paying for a result, not a service. After all, no one wants to purchase scaling and root planning. People want to buy a better oral health future. For this reason, I make my treatment options time bound and make a commitment to them that if they are doing their part that we will add treatment at no additional cost over a predetermined amount of time until we deliver the results they are seeking. I think it is easier for them to commit to treatment when they know we are committed to them.
OARS click to review OARS
“they are paying for a result, not a service”
Service
Scaling and Root Planning have been around for a long time. The diagnosis of the need to remove the substrate that bacteria reside within is independent of the results of the MyPerioPath test. The amount of SRP prescribed does not change based on the results of the test. What does change is the amount of additional and adjunctive therapies recommended. If the patient is found to have high levels of the four bacteria highly associated with systemic health (Aa, Pg, Tf, Td), the dentist might select a treatment protocol that includes systemic antibiotics, general antibacterial treatment of all sulcus and perhaps localized antibiotics in the deepest pockets. What if the patient presents with gingivitis and high-risk pathogens? The approach to disrupt and destroy the high-risk pathogens discovered in gingivitis patients is the same as patients with periodontitis. Only use SRP in areas of attachment loss. We must lessen these bad actors if we want to play our part in reducing systemic inflammation. If they do not have the high-risk pathogens, the dentist will choose a different approach.
Home Care/Support
We know that if the patient doesn’t break up the bacteria every day that grows on their teeth and in their gums, that all our effort will be for naught. Coaching our patients has to be an individualized task. It is unrealistic to ask our patients to change their behavior simply by educating them on the technique and then sending them out into the world to do it and wait three months to see if they got it. We would never accept that of a personal trainer, a running coach or a dietician. We need to customize an engagement strategy to either physically bring them in, talk to them on the phone, text them or whatever works for that patient to ensure that the behavior changes. Remember treatment in the absence of behavior change is just a moment of health. Bob Barkley said: “Health is an interesting thing; the rich can’t buy it and the poor can’t have it given to them.” SRP is the easy part; behavioral change will prove to be the biggest obstacle to positive results. One size fits all will fail most. Frame the problem to the patient well. Next, offer choices. Let them select what they want. Say yes and follow through with your commitment.
“Health is an interesting thing; the rich can’t buy it and the poor can’t have it given to them.” Bob Barkley
Re-evaluation
Physically, we should see the patient if for no other reason than to evaluate their hygiene technique. It is also wise to evaluate the healing of sites and re-administer local antibiotics where needed.
Validation testing
At three months the bacteria counts should be different. The only way to know is to retest a sample of their saliva. On their first periodontal maintenance visit (or better, two weeks before that visit) take another sample and send it in. If the results are good, call them and congratulate them. If the results continue to show a problem, add more care and re-evaluate home care again.
Continued Validation and Monitoring
If you were successful, you need to make sure it doesn’t start over again in the future. Annual testing should be part of the plan.
I tell my patients “I want to give you the right amount of care, nothing more, nothing less.”
You Can Do It!
MyPerioPath is an exciting product that helps us tie the effects of gum disease to overall systemic well-being in a way that has never been possible before. We are swimming in new waters here, and we are not completely sure what lies ahead. These are exciting times to be sure. My fear is that dentists will engage this new technology in a way that is not patient friendly and this could potentially spoil the waters for the rest of the profession. I am a capitalist, and I understand dentistry is a business and decisions must respect marketplace realities. Personally, I believe the upside to the MyPerioPath test is how it can be used to customize treatment and validate success. I do not view it as another service I can sell some patients or use to fight insurance companies. I tell my patients “I want to give you the right amount of care, nothing more, nothing less.” Before the MyPerioPath test, I only had somewhat subjective ways to know how successful I was and I never could validate that their systemic health was not being adversely affected by their oral health. Today that is different. How exciting! Every practitioner has the privilege and the obligation to determine how best to use the knowledge presented in this paper. It is my sincere hope that this will act as the catalyst in your implementation of the new technologies and the time-tested behavioral techniques.
