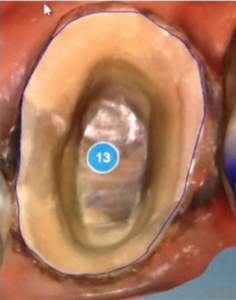
Sloppy Prep

I remember in a basic computer class in grade school where the teacher explained the theory of “Garbage In, Garbage Out.” It seems almost too basic to include on a list of CEREC pitfalls, but the computer can not make a silk purse out of a sow’s ear. A sloppy prep can occur for many different reasons. It is wise to remember the saying “Garbage In, Garbage Out.”
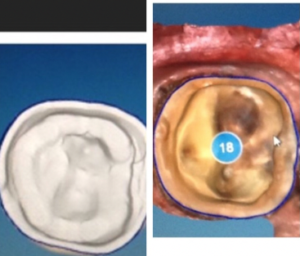
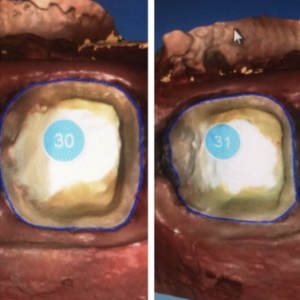
Occlusal reduction


The ideal minimal occlusal reduction depends on the materials, the forces expected to influence the occlusion and the quality of the prep. The adage measure twice cut once, can be modified for CEREC, “Measure twice, the image once.” Know your material, know your force considerations, look at your prep visually, with a known instrument diameter such as a ball burnisher, have the patient squeeze on fast setting bite registration material and measure with an Iwason Gauge, or use flexible clearance guides like the ones from bell de st claire.
Over Reduced Axial Walls
The stronger the clinical crown, the more durable the CEREC crown (assuming ideal reduction.) The point is taking away more tooth can be as damaging to the comfort and long-term outcome of the restoration as taking away too little. Think of Goldie Locks—Just Right. I have seen countless preps where more axial wall reduction and interproximal wall reduction occurs than is necessary. I have had to warranty several crowns that broken off at the gumline not because an issue with ferrule, but rather due to a clinical crown that will never withstand the forces of occlusion. I have also seen times and personally created situations where ferrule became an issue due to my preparation design, not due decay.
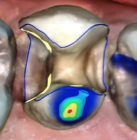
Sharp Line Angles

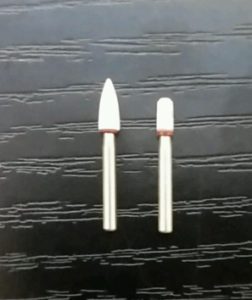
CEREC loves it to be round. It makes sense; a sharp edge will cut and intensify force into a small area. If the force is large enough and the material weak enough that concentration of force will cause a fracture. CEREC has a way of creating a larger cement space around these sharp angles, but I have not figured out how to estimate what that will due to the amount of CEREC material that will live above the internal gauge before the proposal. I guess you could have CEREC create a proposal and then go measure, but now your 90-minute appointment becomes a 120-minute encounter, and every 10 minutes past 90 your patient will dislike you just a little bit more. Round your preps and all will be right.
Of course, this is easier said than done. I love two instruments for this, a Brasseler KS5 and a modified white stone.
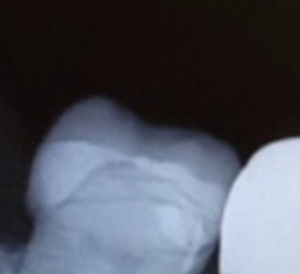
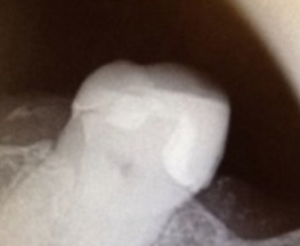
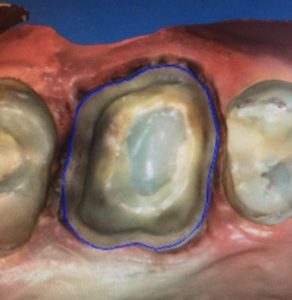
Stepped, Rough, Irregular, Dual, Imperfect Margins.
Perfect margins are like a unicorn, they sound cool, but I have never seen one-I’m not sure they exist. That said, we should do everything in our power to have the best damn margin that your hands can deliver, and that should get better month after month if you implement a deliberate practice strategy.
Inconsistent Reduction
Most dentists have a tendency to slant their preps due to the angulation of the handpiece, the patients head, and even their hand. I have noticed most dentists over reduce the distal and have much greater taper than they have on the mesial. This inconsistent reduction is something to look for in your preps. It takes a long time to improve—I’m going on eighteen years and I still struggle with this.
Margin Placement/ Biologic Width

The CEREC chant goes something like “High and Dry, High and Dry, High and Dry.” I think overall this is a good strategy, but personally, I love mechanical retention, and I am not getting compensated enough for my average crown fee to have thirty different shades and translucencies sitting on my shelf. I am more or less an equigingival margin dentists (other camps, please forgive me.) I look for results, I want a conservative prep, but I want predictable retention, and I never want a patient asking me about a line he can see on the tooth where my A1 meets his A3. So, I choose equigingival margins. If it is deep, I refer for crown lengthening (another camp now hates me.) I believe in biologic width. I believe that it is a number that specific for each patient. I never want to violate biologic width. I also believe in a ferrule. If I can’t get 2 mm of relatively solid buccal wall height and lingual wall height I send the patient out to get it. I don’t just bury the margin because I believe in biologic width. Plus, it is super hard to use CEREC below the gingiva. Make your life easier, grant the patient a better long-term outcome and refer for crown lengthening.
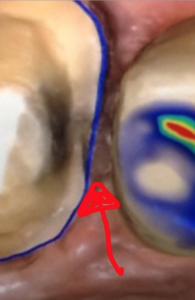
Incomplete Carries Removal
My hope is this isn’t that common, but do your best to make sure all decay is gone. I like carries detection dye, but I know many dentists don’t. It’s your call. Just don’t leave decay.
Undercut
If you do inlays with CEREC, you either figure out undercut issues, or you stop doing inlays. Crowns are different. Depending on your hands you might end up with undercuts. CEREC will compensate for this, but then you get all sorts of weird fluid dynamics involved in your cementation that I don’t pretend to understand. Easier just to round out undercuts and let the cement flow evenly.
Path of Insertion Considerations/ Proximal Teeth Issues

The adjacent teeth don’t always cooperate with our ability to make an excellent fitting crown. Of course, orthodontic therapy would be the best way of handling the issue, but recontouring or even restoring the adjacent teeth might be necessary. Just because you are replacing tooth structure doesn/t mean you are limited to the way the surrounding presents itself. Shoving a tooth in a space that is not easy to maintain is not always in the patients best interests. Take some time and determine what ideal would look like and explain the challenge to your patient. Most patients aren’t willing to go as far as orthodontics, but I have had some pursue this path. My guess is that this was the tipping point to get them to justify the braces they had wanted for some time. Most of the time, I have been able to help the patient see the wisdom in restoring more than one tooth. It goes without saying, do no harm if you haven’t learned how not to gouge the adjacent tooth put a matrix band on the adjacent tooth to protect it.